During his keynote speech at the 22nd Annual Healthcare Summit, Hamed Shahbazi (WELL Health Founder, Chairman & CEO) discussed the collective challenges we face in Canadian healthcare, how WELL is helping to solve those problems, and what WELL believes is the future of healthcare.
Our latest blog recaps elements from Hamed’s speech titled ‘Improving our Healthcare Ecosystem by Better Supporting our Care Providers’ and more.
What is WELL Health?
WELL Health is a physician support and empowerment company. We aim to positively impact health outcomes by leveraging our Practitioner Enablement Platform, to empower and support patients and doctors.
“We’re passionate about how digital tools can introduce efficiencies that give practitioners their time back,” explains Hamed.
But WELL is more than just a technology company. We are also a health system, supporting over 2,300 clinicians in our owned and operated WELL Health Clinic Network. This combination of Platform plus Outpatient Medical Clinics means WELL is uniquely positioned to understand how to support physicians and empower patients.
Challenges in Canadian Healthcare
As Canadians, we are lucky. We have the right to universal healthcare. And that isn’t something anyone should take for granted.
However, it’s clear that Canadian healthcare is facing challenges and that we must make improvements, starting with better supporting our healthcare providers.
Healthcare Challenges at the Clinic Level
The reality is that it takes a lot to manage a clinic. It always has been hard, but with mounting financial pressures adding to pre-existing clinical challenges, it is becoming even harder.
Unless they are part of a network with shared operational and administrative support and resources, clinics will always find it challenging to keep up with new technologies and evolving patient and admin needs and demands. To run successful clinics, our current system asks physicians to do a lot more than just provide care!
Below are some examples of “non-care” related items that are important components of running an outpatient medical clinic.
| Protecting Healthcare Data | Backoffice Payments & Admin | Managing Staffing & HR Performance | Physician Recruitment & Retention | Critical Care Workflows | Managing Billing |
| Managing Clinic IT Requirements | Managing Supply Chain | Regulatory Compliance | Optimizing Workflows | Redundancy That Reduces Patient Risk | Managing Landlords & Leases |
Increasingly, factors such as rising lease costs and supply chain challenges, are piling even more pressure on clinics, distracting physician time and resources away from care delivery.
Meeting patient expectations after the introduction of technology implemented during the pandemic is also a challenge, as patients have begun to appreciate the flexibility of digital experiences like telehealth and online booking.
Ultimately, if clinics can’t stay profitable, physicians are forced to consider closing their doors. And if a clinic closes, it affects access to healthcare in the community.
Digitizing clinics is hard, and most doctors aren’t technologists. More support for physicians at the clinical level, allowing doctors to focus more of their time on care is desperately needed.
Collective Healthcare Challenges
We’ve looked at the challenges that individual clinics face, but there are collective challenges that we – as Canadians – also face. These are factors that also impact our Canadian healthcare system, but the solution to these problems goes far beyond any one physician or clinic.
-
Family Doctor Shortages
Family doctors are the backbone of our healthcare system as they provide longstanding care in our communities.
But the number of Canadians aged 12 and older without a regular doctor is around 4.6 million. If the shortage of family doctors continues, in Ontario, alone, that number could reach 3 million by 2025.
-
Fewer Doctors are Choosing Family Medicine
Insufficient support and resources and too much administration are disincentives for doctors to enter (or remain in) family medicine. The College of Family Physicians of Canada state that fewer medical school graduates are choosing family medicine due in part to stagnant payment models and rising costs.
We can’t take family doctors for granted. We need to get behind them and provide greater support to our care providers.
-
Access to Timely Care
The downstream impact of the mounting pressure on clinics as well as family doctor shortages is more and more Canadians not being able to access timely care. Around 50% of patients say they have difficulty getting a same or next-day appointment with a physician, even with their own family doctor.
When patients can’t access timely care, they often look to the emergency room for care. This places additional strain on ERs and these trips cost taxpayers considerably more than primary care visits, increasing overall costs to Canadians.
-
Lack of Digitization
Health as a sector is very under-digitized compared to almost every other aspect of our lives.
A 2019 study of primary care physicians in 11 high-income countries found that only 20% of Canadian doctors offered online booking options. Canada also ranked last for digital test results and prescription refills. Increased digitization creates better experiences for both physicians and patients.
What are Canadian physicians saying?
With all these challenges, what are physicians in Canada telling us? What are the lessons we can, and should, learn from their experiences?
Well, through national surveys, we know that physicians and clinic teams in Canada spend on average 50% of their time on administration. And over half of Canadian physicians attribute burnout to manual tasks like charting and paperwork.
Preliminary data from the CMA’s National Physician Survey revealed that:
- 59% of physicians indicated their mental health has worsened since the start of the COVID-19 pandemic
- Over 50% of physicians point to the increased workload and changing policies and processes as reasons for the negative impact on their mental health
All this leads to less time being spent with patients, which means less time providing care. Or worse, it means doctors cutting back on their hours or leaving the public system completely due to burnout.
At WELL, increasingly we are finding that doctors don’t want to run their own businesses anymore. They want support, in terms of both tools and resources so they can focus on care.
What is WELL doing to help?
At WELL Health, we’re focusing on caring for our carers. We can do that in many ways, but the priority is digitization.
By digitizing healthcare in Canada, we can optimize physician time. That means less paperwork and manual processes that we know cause burnout. Digitization empowers physicians to spend more time providing care.
Ultimately, if we digitize healthcare, our physicians will feel more fulfilled and efficient. There are approximately 90,000 physicians in Canada. If WELL Health can save every physician even 10% of their time, that is equivalent to adding thousands of additional physicians to our healthcare system.
That isn’t to say Canadian physicians are inefficient, they are working incredibly hard to provide care in their communities. But they are facing too many challenges, meaning less time is focused on care and leading to more physicians feeling burnt out.
So that’s what we want to do! We want to help support teams so they can help doctors. And we want to support doctors so they can care for Canadians.
Let’s look at the two ways that WELL Health is working to support physicians.
Both options allow physicians to access WELL Health’s practitioner enablement platform, including well-known services like Ocean and DoctorCare.
With WELL’s practitioner enablement platform, physicians (and their support staff) can optimize their time.
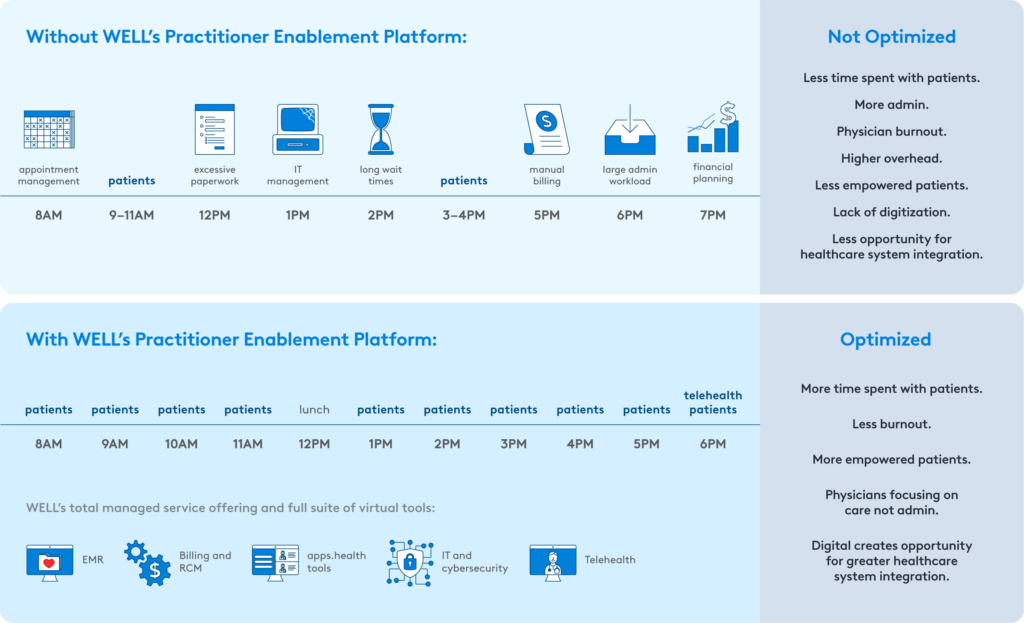
We’re giving doctors their time back. This is time that could be used for preventative care.
WELL’s practitioner enablement platform features trusted, physician-approved digital tools and services that integrate with OSCAR Pro. Direct integration is a crucial feature, as it is this automated flow of information that allows physicians and their support staff to move away from manual administration.
Let’s look at two examples of tools in our Practitioner Enablement Platform, Ocean and Tali.ai. Both serve as great examples of how physicians can benefit from digitization.
Ocean
Ocean is a leading patient engagement platform that connects patients and healthcare providers using secure patient forms, screening tools, and surveys that integrate with the EMR.
From online booking to self check-in tablets in the waiting room and online patient registration, we know that Ocean is making a difference in the battle to digitize and automate in-clinic administration.
Ocean now reaches over 800, 000 patient encounters each month. And patients appreciate the difference, with over 95% of patients who encounter Ocean reporting that it provides a better experience.
Tali
Tali is a voice-enabled virtual assistant that transcribes a physician’s voice commands replacing manual data entry. This solution quickly and accurately scribes for physicians and is well-versed in terminology and abbreviations.
Tali saves physicians as much as 10 hours a week, significantly easing administrative burdens that lead to burnout. These are the kinds of tools that the WELL Clinic Network is providing to physicians.
Both Ocean and Tali are also available to non-WELL clinics through apps.health.
The Future of Healthcare is Open and Connected
The patient journey can be complex, but digitization helps improve both patient and practitioner experiences.

apps.health, our hub for digital health innovation, is designed for all of WELL’s many thousands of EMR customers. OSCAR Pro users can choose from 40+ integrated digital apps and services designed to improve efficiency and health outcomes.
The innovative solutions available on apps.health also solve problems for patients. Through integration between OSCAR Pro and Apple Health, we are empowering patients with access to their personal health information via the Apple Health app. Armed with their personal health information, patients can become more active participants in their own care.
At The Heart of Healthcare
We are helping practitioners do what they do best – care for their patients. From dealing directly with healthcare providers and offering innovative technologies so they can deliver exceptional care, to helping patients secure their own healthcare data, we are focused on making a meaningful and positive difference.
You can read about WELL’s vision, commitments, and priorities in WELL’s 2021 ESG Report. Or, to learn about our Practitioner Enablement Platform, visit well.company

